A group of researchers has developed an entirely novel approach to treating eating disorders.
The scientists showed that a group of nerve cells in the hypothalamus (so-called AgRP, agouti-related peptide neurons) control the release of endogenous lysophospholipids, which in turn control the excitability of nerve cells in the cerebral cortex, which stimulates food intake. In this process, the crucial step of the signaling pathway is controlled by the enzyme autotaxin, which is responsible for the production of lysophosphatidic acid (LPA) in the brain as a modulator of network activity.
The administration of autotaxin inhibitors can thereby significantly reduce both excessive food intake after fasting and obesity in animal models. The article, "AgRP neurons control food intake behavior at cortical synapses via peripherally-derived lysophospholipids" appeared in Nature Metabolism.
Eating disorders and especially obesity are one of the most common causes of a variety of diseases in industrialized societies worldwide, especially cardiovascular diseases with permanent disabilities or fatal outcomes such as heart attacks, diabetes, or strokes. The Robert Koch Institute reported in 2021 that 67 percent of men and 53 percent of women in Germany are overweight; 23 percent of adults are severely overweight (obese). Attempts to influence eating behavior with medication have so far proved ineffective. A novel therapy that modulates the excitability of networks that control eating behavior would be a decisive step towards controlling this widespread obesity.
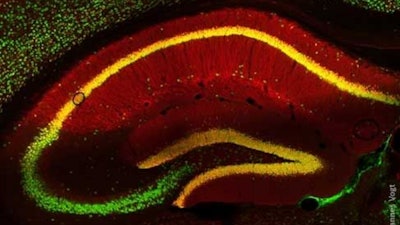
The research team found an increased rate of obesity and the attendant type II diabetes in people with impaired synaptic LPA signaling. A group led by Professor Johannes Vogt (Faculty of Medicine, University of Cologne), Professor Robert Nitsch (Faculty of Medicine, University of Münster) und Professor Thomas Horvath (Yale School of Medicine) has now shown that control of the excitability of neurons in the cerebral cortex by LPA plays an essential role in the control of eating behavior: AgRP neurons regulate the amount of lysophosphatidylcholine (LPC) in the blood. Through active transport, LPC reaches the brain, where it is converted by the enzyme autotaxin (ATX) into LPA, which is active at the synapse. Synaptic LPA signals stimulate specific networks in the brain, thus leading to increased food intake.
In the mouse model, after a period of fasting an increase in LPC in the blood led to an increase in stimulating LPA in the brain. These mice showed typical food-seeking behavior. Both could be normalized by administrating autotaxin inhibitors. Obese mice, on the other hand, lost weight when these inhibitors were administered continuously.
Vogt explained, "We saw a significant reduction in excessive food intake and obesity through gene mutation and pharmacological inhibition of ATX. Our fundamental findings on the LPA-controlled excitability of the brain, which we have worked on for years, therefore also play a central role for eating behavior."
Robert Nitsch sees the findings as an important step towards new drug development.
"The data show that people with a disturbed synaptic LPA signaling pathway are more likely to be overweight and suffer from Type 2 diabetes. This is a strong indication of a possible therapeutic success of ATX inhibitors, which we are currently developing together with the Hans Knöll Institute in Jena for use in humans."
These findings on the excitation control of neuronal networks in eating behavior through lysophospholipids and the new therapeutic possibilities they suggest could in future contribute not only to treating eating disorders, but also neurological and psychiatric illnesses.






















